Uterine cancer, the most prevalent gynecologic cancer in the United States, has seen a concerning rise in recent years. Disturbingly, there's currently no standard screening method for this disease, which is projected to affect approximately 66,200 women and claim the lives of around 13,000 in 2023, according to the American Cancer Society (ACS).
Dr. Brian Slomovitz, a leading gynecologic oncologist at Mount Sinai Medical Center in Miami Beach, Florida, and chair of the Uterine Cancer Awareness Month initiative, highlights this alarming trend. While overall cancer rates are declining, uterine cancer cases are unfortunately increasing, and deaths from this disease are predicted to soon surpass those from ovarian cancer.

Although the terms "uterine cancer" and "endometrial cancer" are often used synonymously, there's a subtle distinction. Endometrial cancer refers specifically to cancers originating in the uterine lining (endometrium), which account for the vast majority of cases. Uterine sarcomas, impacting the uterine muscle, represent a smaller percentage but are significantly more aggressive.
Obesity stands out as the most significant risk factor for uterine cancer. Excess fat tissue elevates estrogen levels, and endometrial cancer thrives in high-estrogen environments. The ACS indicates that overweight women have double the risk, while obese women face triple the risk, compared to women at a healthy weight. Diabetes, often linked to obesity, also increases the risk.
Other risk factors include polycystic ovarian syndrome (PCOS), which disrupts hormone balance, and certain hereditary conditions like Lynch syndrome. Age is another factor, with most diagnoses occurring in women in their 50s and 60s.

Abnormal bleeding is the most common symptom of uterine cancer, particularly postmenopausal bleeding. However, recognizing abnormal bleeding can be challenging for premenopausal women. Other symptoms may include pelvic pain or pressure. Given the lack of routine screening, prompt medical attention for persistent symptoms is crucial.
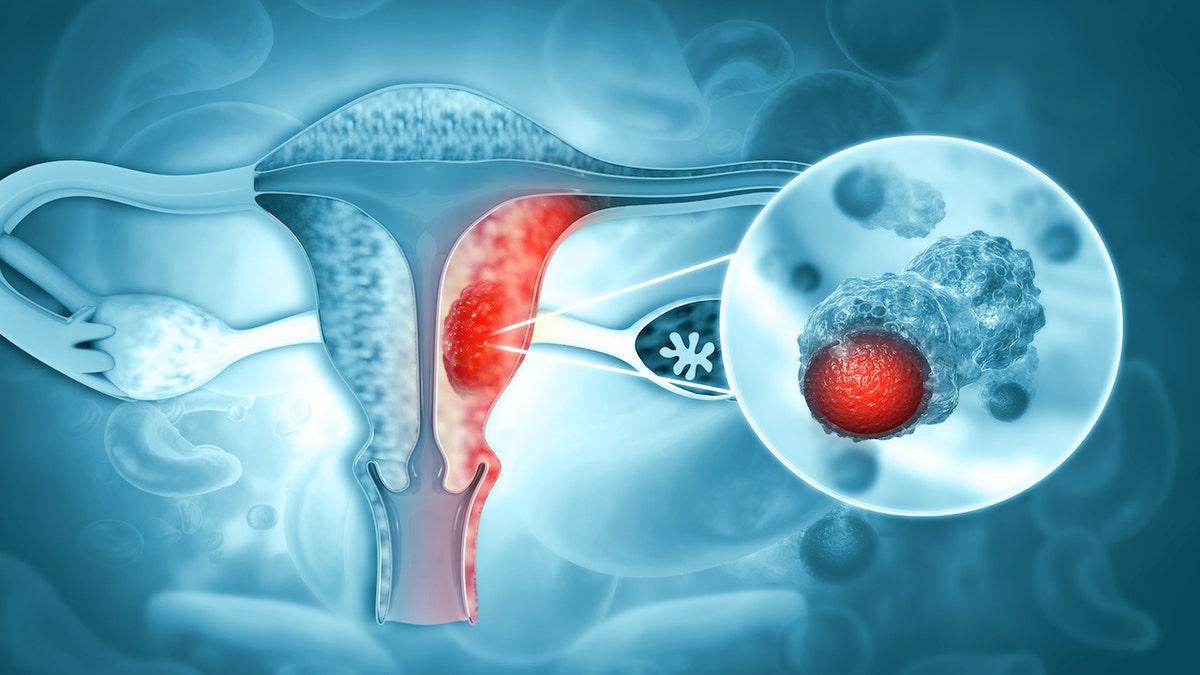
Diagnosis typically involves an ultrasound followed by a tissue biopsy. Advanced cases may require further imaging tests like X-rays, CT scans, MRIs, or PET scans to assess the extent of the disease's spread.

Hysterectomy, the surgical removal of the uterus, is a common initial treatment, boasting an 80% cure rate. Lymph node sampling is often performed concurrently to check for cancer spread. For advanced or recurrent cases, systemic therapies like chemotherapy or hormonal therapy are employed.

Promising new treatments, including immunotherapy and antibody-drug conjugates (ADCs), offer hope for improved outcomes in aggressive cases. Molecular classification, which categorizes uterine cancers into subtypes, is also paving the way for more personalized treatment strategies. These advancements represent a significant step towards improving survival rates and quality of life for women battling this disease.

Comments(0)
Top Comments